Filling out the New York Do Not Resuscitate (DNR) Order form is a critical step for individuals wishing to communicate their healthcare preferences. However, several common mistakes can occur during this process, potentially leading to confusion or unintended consequences. Understanding these pitfalls can help ensure that the form accurately reflects the individual's wishes.
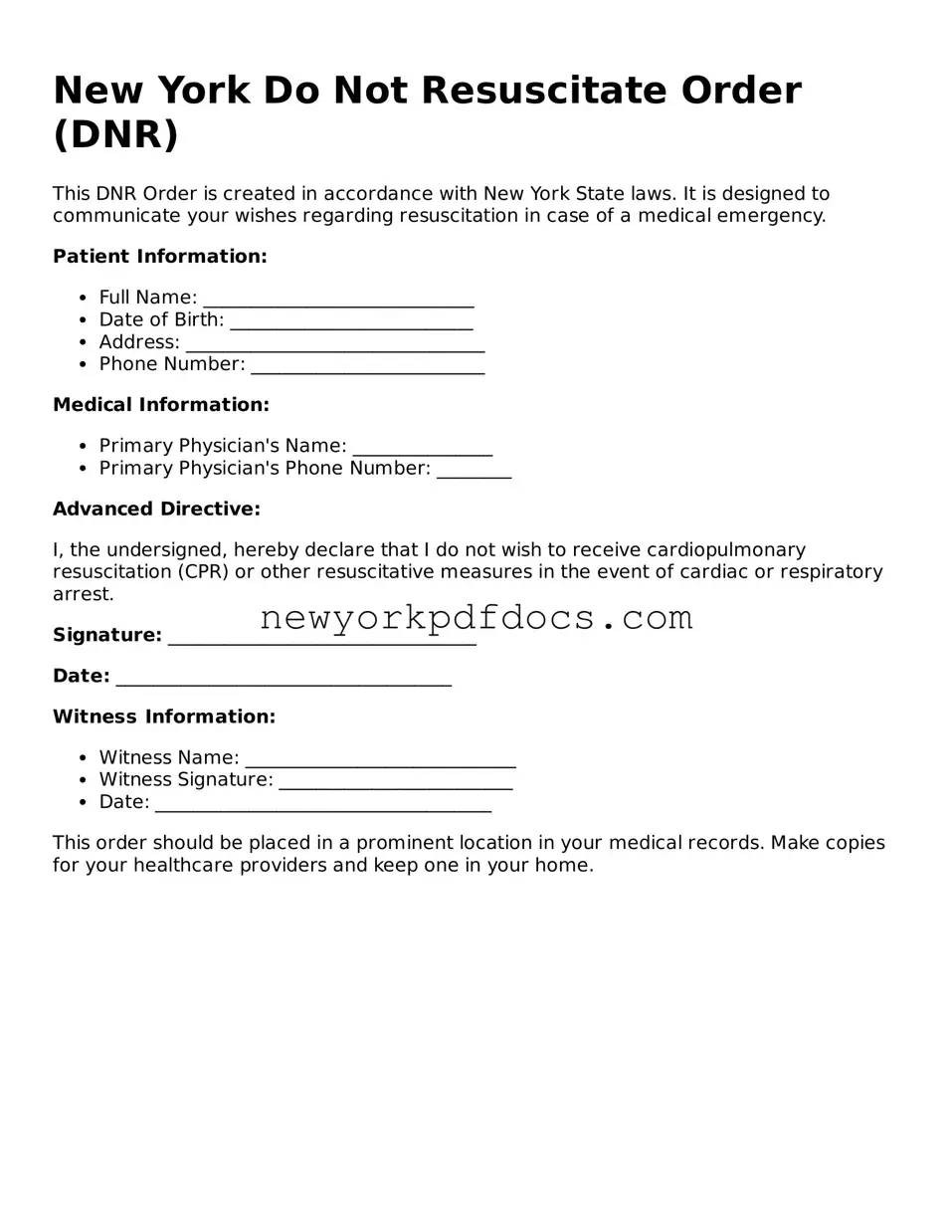
One frequent error is failing to provide complete personal information. The form requires specific details, such as the patient's full name, date of birth, and address. Omitting any of this information can result in the form being deemed invalid. It is essential to double-check that all fields are filled out correctly before submission.
Another mistake involves not signing the form properly. The DNR Order must be signed by the patient or their legally authorized representative. If the signature is missing or not dated, healthcare providers may not recognize the document as valid. Ensuring that the signature is clear and accompanied by the date is crucial.
Some individuals overlook the importance of having the form witnessed. In New York, the DNR Order must be signed in the presence of two witnesses, who also need to sign the document. Failing to include witnesses can render the form ineffective. Witnesses should be impartial and not related to the patient, ensuring an unbiased validation of the document.
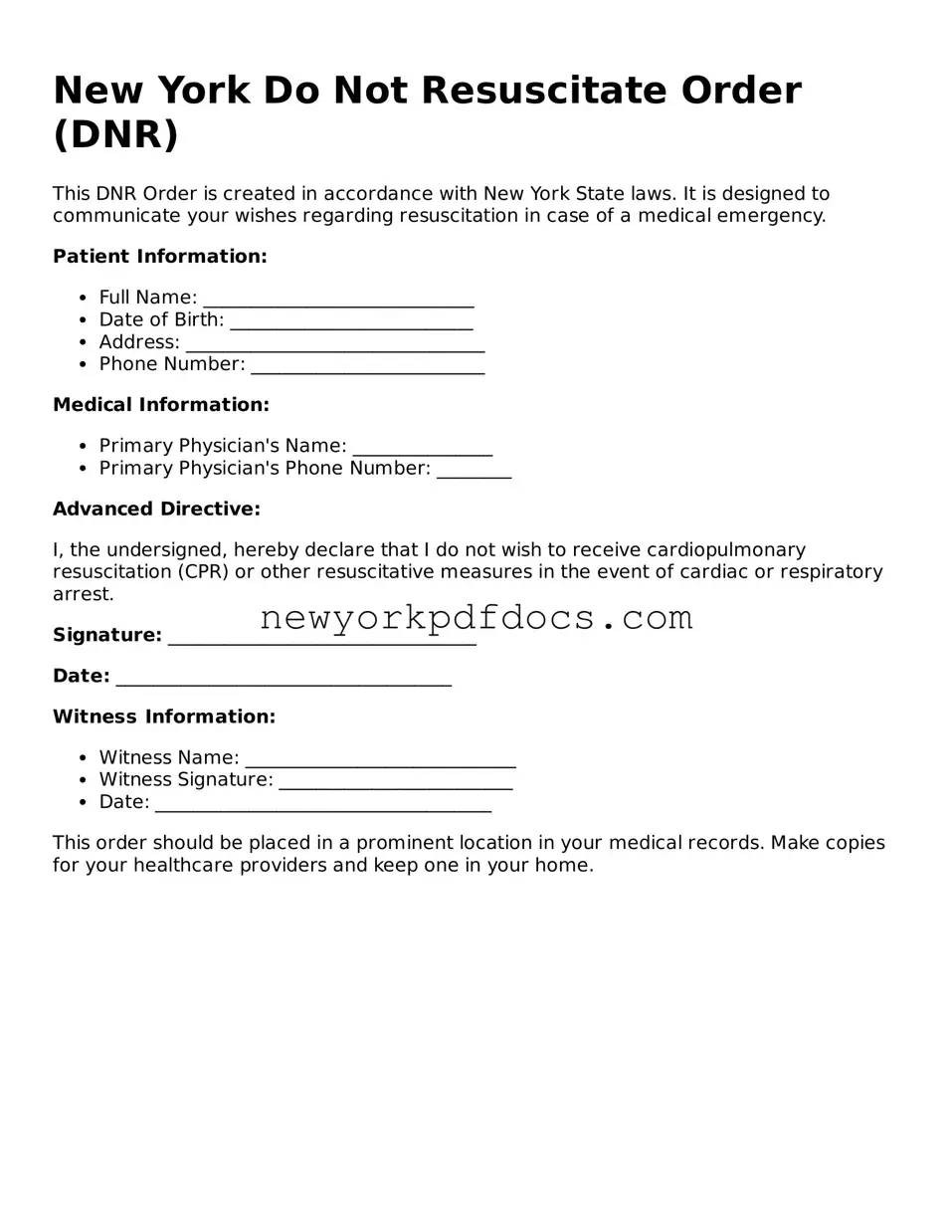
Additionally, people sometimes misunderstand the scope of the DNR Order. It is vital to recognize that this document specifically addresses resuscitation efforts in the event of cardiac or respiratory arrest. Some individuals mistakenly believe that a DNR Order applies to all medical treatment, which is not the case. Clarifying this distinction can prevent misinterpretations of the patient's wishes.
Another common mistake is neglecting to communicate the existence of the DNR Order to family members and healthcare providers. Even if the form is filled out correctly, failing to inform relevant parties can lead to confusion during a medical emergency. It is advisable to share the DNR Order with family members and ensure that healthcare providers have access to it.
Lastly, individuals may not keep the DNR Order in an accessible location. The form should be stored where it can be easily found by medical personnel during an emergency. Keeping copies in multiple locations, such as with a primary care physician and at home, can help ensure that the patient's wishes are honored when needed.